Will pancreatitis complicate my efforts to secure life insurance?
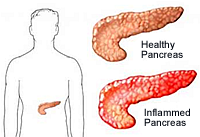
Pancreatitis means inflammation of the pancreas, an elongated gland that is located behind the stomach. It is a condition that can be acute or chronic and affects men more often than women.
Two Types of Pancreatitis
Other related medical conditions (or medical terminology) include Pancreatitis, Acute Pancreatitis, Chronic Pancreatitis. Read below for more information about Pancreatitis and receiving a life insurance quote from a life insurance specialist.
Acute Pancreatitis
Acute pancreatitis in adults can be caused by gallstones, gallbladder disease and alcohol use. It can also be brought on by viral infections, traumatic injuries, pancreatic or common bile duct procedures or medications. In some instances, the condition may be caused by the abnormal structure of the pancreas, hypertriglyceridemia (elevated lipid levels in the blood), heredity or complications from cystic fibrosis. Children may experience this condition as a result of abdominal trauma, cystic fibrosis, hemolytic uremic syndrome, Kawasaki disease, mumps, Reye syndrome, viral illnesses or medications.
A person should suspect acute pancreatitis if they have persistent or chronic upper left quadrant pain or upper middle of the abdomen. It may radiate to the back or below the left shoulder blade. The pain often becomes worse when lying flat on the back or after eating fatty foods or drinking. Alcohol consumption may heighten the pain. In addition to the acute pain, a person suffering from pancreatitis may experience nausea, vomiting, sweating, anxiety, fever or mild jaundice. The abdomen may appear swollen. Hiccups, abdominal indigestion and skin rash may occur. Stools may become clay colored.
If pancreatitis is suspected following a general examination, the doctor may request blood work to check for elevated levels of glucose, serum amylase, urine amylase, serum lipase and white blood count (WBC). Serum calcium levels may be decreased. They may order an abdominal CT scan, ultrasound or MRI to detect inflammation of the organ. Results from testing will indicate a course of treatment. If gallstones, obstructions of the pancreatic ducts or fluid collection around the pancreas are the suspected cause, radiologic or endoscopic therapy may be utilized. In severe cases, when the pancreas has scarring or fibrosis, surgery may be required to remove dead, infected tissue.
The prognosis for acute pancreatitis can vary. Most cases resolve in a about a week, however, some cases may become life-threatening and complications such as liver, heart or kidney impairment may happen. Recurrences of pancreatitis are not uncommon.
Chronic Pancreatitis
As with acute cases, chronic pancreatitis occurs when there is ongoing inflammation of the pancreas. Over time, scarring of tissue in the pancreas prevents it from producing adequate amounts of enzymes to digest fat. This constant inflammation also interferes with the production of insulin, which may lead to diabetes.
Chronic pancreatitis mimics acute attacks with regard to pain symptoms. It differs in the duration of the abdominal pains and digestive problems which may last hours, days or longer. Sitting up and leaning forward may temporarily relieve pain symptoms. Unintentional weight loss may result can be a warning signal.
Blood work from individuals with chronic pancreatitis may show elevations in serum lipase and serum amylase, but the elevations may return to normal as the disease progresses. Levels of serum trypsinogen may be low and fecal fat tests will reveal fatty stools. An abdominal CT scan or ultrasound may be ordered. An endoscopic retrograde cholangiopancreatography (ERCP), a procedure performed with an endoscope to identify stones, tumors, or narrowing in the bile ducts or exploratory laparotomy may be done to confirm the diagnosis.
The cause of this condition is often alcohol abuse and alcoholism, though sometimes the cause may not be determined. Other illnesses that are often linked to chronic pancreatitis include hyperlipidemia or hyperparathyroidism, injury and chronic blockage of the pancreatic duct.
Treating Acute and Chronic Pancreatitis
Treatment plans and goals for acute and chronic pancreatitis patients differ. For individuals suffering from an acute episode, treatment is aimed at pain relief. Intravenous (IV) infusion may be administered to address fluid loss, while food or fluid by mouth may be withheld to limit the activity of the pancreas. Nasogastric suctioning may be required when a person has persistent vomiting or severe pain. Similarly, the goal of treatment for chronic pancreatitis is also pain relief. Diabetes must be treated if it is a factor. Nutritional recommendations include a low fat diet along with the addition of fat soluble vitamins and calcium. Pain relief medication or a surgical nerve block may be administered as well as supplemental pancreatic enzymes to correct underproduction. Insulin might be prescribed to control blood sugar levels. Surgery may be required if a blockage is identified, or if part, or all, of the pancreas is irreparably damaged.
Pancreatitis and alcohol do not mix. Individuals who have suffered an acute attack are warned to avoid heavy consumption of alcohol, whereas chronic sufferers should avoid alcohol altogether.
Pancreatitis and Insurability
When the cause of an acute pancreatitis attack is gallstones, or another identifiable medical event, insurers will want to wait for the applicant to be fully recovered and without symptoms for several weeks before accepting an application. In instances where a person has had several acute attacks, without any known cause, an insurer will want to rule out alcohol abuse. If alcohol can be eliminated as a possible cause, and a pre-determined period of time has passed without another pancreatitis incident, then an insurance application will proceed as normal. When several acute episodes are due to a known cause, such as gallstones, insurance opportunities will reflect how well the condition can be controlled, normally opting to postpone a decision until the cause of the pancreatitis can be managed or eliminated.
How Can MEG Financial Help?
At MEG Financial, we have worked with many individuals across the country that have had alcohol related histories and have helped many obtain fairly priced life insurance. A number of these clients previously attempted to buy life insurance elsewhere but were either turned down or asked to pay a significantly higher rate. Our experience helping others with alcohol related problems is invaluable to you in identifying the insurance company that will treat you most fairly.
For more specific information or to obtain a custom quote, call MEG Financial today at (877) 583-3955. You may also submit this short form and an independent insurance agent will personally contact you to go over any questions or other concerns.

 Speak with an experienced advisor!
Speak with an experienced advisor! 


